- Plantar Fasciitis (PF)
- Causes of Plantar Fasciitis
- Symptoms of Plantar Fasciitis
- Diagnosis of Plantar Fasciitis
- Plantar Fasciitis Prevention
- Treatment for Plantar Fasciitis
- Nonsurgical Treatment
- Orthoses
- Steroid Injections
- Extracorporeal Shockwave Therapy
- Plantar Fasciotomy surgery
- Gastrocnemius Recession surgery
- MANOS Plantar Facia Release System
Plantar Fasciitis (PF)
Plantar fasciitis occurs when the band of tissue that supports the arch of your foot becomes irritated and inflamed. The plantar fascia is a long, thin ligament that lies directly beneath the skin on the bottom of your foot. It connects the heel to the front of your foot, and supports the arch of your foot. The plantar fascia is designed to absorb the high stresses and strains we place on our feet. Excessive pressure can damage or tears the tissues. The body's natural response to injury is inflammation, which results in the heel pain and stiffness of plantar fasciitis.

Causes of Plantar Fasciitis
In most cases, plantar fasciitis develops without a specific, identifiable reason. There are, however, many factors that are associated with the condition:
- Tighter calf muscles that make it difficult to flex your foot and bring your toes up toward your shin
- Obesity
- Very high arch
- Repetitive impact activity (running/sports)
- New or increased activity
Although many people with plantar fasciitis have heel spurs, spurs are not the cause of plantar fasciitis pain. One out of 10 people has heel spurs, but only 1 out of 20 people (5%) with heel spurs has foot pain. Because the spur is not the cause of plantar fasciitis, the pain can be treated without removing the spur.
Symptoms of Plantar Fasciitis
The most common symptoms of plantar fasciitis include:
- Pain on the bottom of the foot near the heel
- Pain with the first few steps after getting out of bed in the
morning, or after a long period of rest, such as after a long car ride.
The pain subsides after a few minutes of walking - Greater pain after (not during) exercise or activity
Diagnosis of Plantar Fasciitis
Plantar fasciitis is typically diagnosed by clinical examination. A detailed patient history including medical conditions, work history, and prior foot/ankle injuries is important The physician may decide to use imaging studies like radiographs (X-rays), diagnostic ultrasound and MRI.
 Heel spurs, a small bony calcification on the calcaneus heel bone, are often associated with this condition. It is the underlying plantar fasciitis that causes the pain, not the spur itself. The condition is responsible for the creation of a heel spur, but the plantar fasciitis is not caused by the spur.
Heel spurs, a small bony calcification on the calcaneus heel bone, are often associated with this condition. It is the underlying plantar fasciitis that causes the pain, not the spur itself. The condition is responsible for the creation of a heel spur, but the plantar fasciitis is not caused by the spur.
Plantar Fasciitis Prevention
These steps will help prevent plantar fasciitis:
Maintain a healthy weight
Warm up and stretch before participating in sports
Wear shoes that support the arch and cushion the heel.
For people prone to episodes of plantar fasciitis, exercises that stretch the heel cord (the Achilles tendon) and the plantar fascia may help prevent plantar fasciitis from returning. Ice massage also can be used on the bottom of the foot after stressful athletic activities.
Treatment for Plantar Fasciitis
Conservative care is effective for the majority of PF patients. However, patients with refractory PF do not have ideal solutions to treat their ongoing symptoms.
Plantar stretching is the primary initial treatment regimen and significant long-term improvement (10+ months) is experienced in the majority of patients. For patients who do not respond to stretching, orthotics can improve pain levels.
Non-surgical interventions have not proven to be effective as a long-term treatment strategy. Extracorporeal shockwave therapy (ESWT) shows equivocal benefit with some studies showing significant improvement and others showing none. Steroid therapy, when coupled with plantar stretching, can provide efficacious pain relief. However, they have been shown to be no better than a placebo at 3 months.
Plantar fascia release surgery is commonly employed as the definitive treatment for PF. However, the length of recovery limits the surgery to a bail-out strategy when conservative measures have failed.
Nonsurgical Treatment
Plantar fasciitis is aggravated by tight muscles in the feet and calves. Stretching the calves and plantar fascia is the most effective way to relieve the pain that comes with this condition.
Orthoses
When rest and stretching have failed to improve PF symptoms, orthotics are typically the next level of treatment. Shoes with thick soles and extra cushioning can reduce pain with standing and walking. As you step and your heel strikes the ground, a significant amount of tension is placed on the fascia, which causes microtrauma (tiny tears in the tissue). A cushioned shoe or insert reduces this tension and the microtrauma that occurs with every step. Soft silicone heel pads are inexpensive and work by elevating and cushioning your heel. Pre-made or custom orthotics (shoe inserts) are also helpful.
Steroid Injections
Cortisone, or other steroids, is commonly injected into the plantar fascia to reduce inflammation and pain. At least 25% of patients with PF receive steroid injections, despite the limited long term clinical benefit described in the literature.
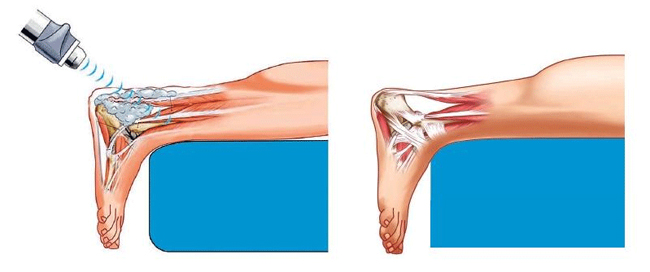
Extracorporeal Shockwave Therapy
Extracorporeal shock wave therapy (ESWT) has emerged as a possible treatment option for patients with chronic plantar fasciitis. ESWT delivers focused shock waves to the body. There is both a high-energy and low-energy form of ESWT, and both forms of shock wave therapy can be used in the treatment of plantar fasciitis.
Shock wave therapy is thought to work by inducing microtrauma to the tissue that is affected by plantar fasciitis. This microtrauma initiates a healing response by the body. This healing response causes blood vessel formation and increased delivery of nutrients to the affected area. The microtrauma is thought to stimulate a repair process and relieve the symptoms of plantar fasciitis.
Plantar Fasciotomy Surgery
Plantar fasciotomy is currently the most common surgical treatment for refractory fasciitis. During surgery, the plantar fascia ligament is partially cut to relieve tension in the tissue. If there is a large bone spur, it can be removed, as well. However, the bone spur is not considered to be a pain generator. Orthopedic foot and ankle specialists and podiatrists perform plantar fasciotomy.
Approximately one third of the surgeries are performed utilizing a minimally invasive, endoscopic technique. However, the traditional approach to plantar fascial release is an open surgical procedure, which can be associated with a prolonged recovery period, often requiring the patient to remain nonambulatory for a period of 4 to 6 weeks with a gradual return to full activity for an additional 8 weeks. Also, the plantar incision can lead to postoperative scarring that can, itself, cause chronic pain and limit function.
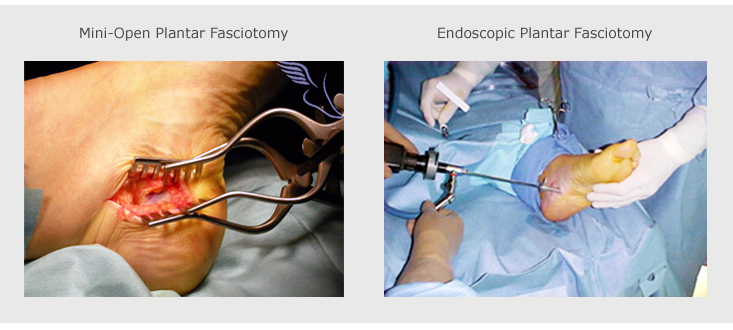
According to the PearlDiver Patient Record Database, surgical release treatments have experienced a relatively steady growth rate of 35% since 2004. Though podiatry still dominates the market with lower cost products such as anti inflammatory medicine and cortisone injections, 100,000 patients are presently undergoing surgical release treatments every year.
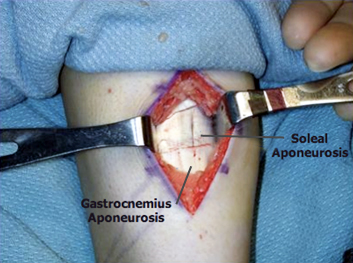
Gastrocnemius Recession Surgery
Gastrocnemius recession is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the plantar fascia, this procedure is useful for patients who still have difficulty flexing their feet.
In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope.
MANOS Plantar Facia Release System
The latest advancement in plantar facia release technology, the MANOS™ Plantar Facia Release System gives patients the option to release the plantar fascia ligament (PFL) through surgical access measuring as little as 2mm. Through this access to the plantar facia ligament, the surgeon releases the PFL with the MANOS cutting surface. The MANOS cutting surface is exposed only after the surgeon first safely positions the device. While positioning the device, MANOS is completely blunt and compatible with nerve stimulation guidance and ultrasound guidance. The entire procedure is performed in about ten minutes.
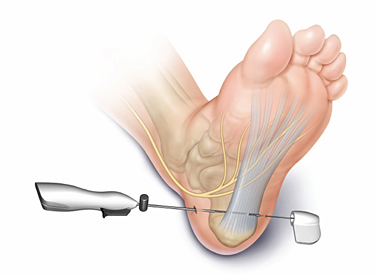
After the procedure, two small band-aids may be used to cover the surgical access points. The procedure is designed to minimize surgical trauma and reduce patient recovery time. Because surgical access is so small, stitches are not normally required and scarring is minimized or eliminated altogether. MANOS PFR patients typically recover relatively quickly, with some patients returning to work as early as the same week of surgery. Postoperative care is limited and generally does not include splinting or physical therapy. Click here to find a MANOS PFR surgeon near you.